A Hidden Post-Pandemic Increase in the Decline of Female Health
by Carla Peeters at Brownstone Institute
As women used to live longer than men even during severe famines and epidemics, a continued post-pandemic increase in female mortality and disabilities can’t stay hidden or neglected.
During the Covid pandemic in many High-Income Countries, injuries, disabilities, and all-cause mortality started to rise above expectations. In 2020, the gender gap in mortality widened due to an observed increased mortality in men. While in 2021 male health seemed to bounce back to earlier trends, mortality and disabilities in women continue to rise above earlier trends and are not expected to solve themselves soon. This might cause a fundamental and permanent change in the dynamics of the gender mortality gap.
Recent decisions on austerity measures for budgets on female health and welfare will exacerbate this hidden disaster. Instead, Public Health Experts and CEOs of insurance companies need to take their moral responsibility and turn to smart investments in female health, addressing all gender disparities, to reverse a downward spiral in global population health.
A Sudden Rise in Excess Mortality and Disabilities
In September 2024, Swiss Re published in their annual report, “Many countries worldwide still report elevated death in their population today.” This impact appears independent of healthcare system or population health. In the pessimistic model, Swiss Re would expect excess deaths to continue for another decade. There is also likely a degree of excess mortality underreporting.
CFOs from other life insurance companies confirmed that experienced mortality rates are broadly in line with this report. A skyrocketing increase in disability claimants since 2020 is another puzzling factor why CEOs of insurance companies are facing major problems with their financial model. The growth in demand is much lower, and the number of people making claims is much higher than expected. Declining revenues may soon hit the corporate bottom line.
For the first time in 80 years, the stocks from insurer Centene Medicaid plummeted in July 2025 by 41% after the insurer had to withdraw its full financial guidance because previous estimates were way off.
The analysis from insurance companies is comparable with earlier reports from Phinance Technologies, which analyzed publicly available data from the US and UK using various methods. Other independent analysts observed similar trends.
In recent years, hundreds of peer–reviewed articles discuss excess mortality and adverse events of special interest in various countries of pandemic measurements and after Covid-19 vaccinations.
Boston University just published the all-cause mortality in the US as compared to other High-Income Countries and showed that excess death rates peaked in 2021 and declined in 2022 and 2023 but remained substantially higher than pre-pandemic rates, especially in the age group 25-44 years. Mortality among US adults aged 25-44 years was 2.6 times higher as compared to other High-Income Countries.
A recent opinion from Kakeya et al. describes a significant increase in excess deaths after repeated Covid-19 vaccinations. Japan is the country with the highest per capita rate of messenger ribonucleic acid mRNA vaccination doses in the world.
A systematic review on Covid-19 mechanisms of injury and death compiled with autopsy confirmation by a physician application suggests there is a likelihood of a causal link between Covid-19 vaccines and deaths.
While there are studies that conclude there is no significant increase in stillbirths when women were vaccinated with the Covid-19 mRNA vaccine during pregnancy, a study based on VAERS data shows a significant increase. Another, not yet peer-reviewed, study indicates that Covid-19 vaccination with dose 1 during weeks 8-13 of pregnancy was associated with 3.9 fetal losses above expected for every 100 exposed pregnancies.
A study in the Czech Republic on live births of vaccinated versus non-vaccinated women demonstrated a substantially lower successful conception rate among vaccinated women than for those who were not vaccinated. The fertility rate in the Czech Republic dropped from 1.85 births per 1,000 women in 2021 to 1.62 in 2022 and 1.45 in 2023. Births in the EU fell to 1.38 births per woman. Also the US reported a historically low birth rate in 2023. Many Western countries are facing a similar problem with dropping fertility rates as the health of young women declined during the pandemic and post-pandemic economic instability.
Furthermore, maternal mortality rates accelerated at an alarming rate, especially from 2019-2022 in the US and UK, mainly caused by cardiovascular problems. The sharp spike in maternal death could not be explained by older age. Pregnancy-related maternal deaths are getting worse. In the UK, suicide remains the leading cause of direct maternal death in the first postnatal year.
Pandemic measures resulted in a collapse of women’s health and income, especially for those with the lowest wages working in healthcare, social services, education, and retail. During this period, the number of female healthcare worker suicides and fatal overdoses increased. ‘When the health of those who look out for people’s health is at risk the whole population and economy are at risk.’
Furthermore, it is well known that women respond more strongly and may experience a higher risk for complications after vaccinations. Observations from vaccination trials in Guinea-Bissau suggest increased female-male mortality ratio associated with inactivated polio and diphtheria-tetanus-pertussis vaccine. There is precedent for the observation that infant girls experience increased mortality following receipt of vaccines. People in healthcare (80% women) have been recommended and sometimes mandated a yearly flu vaccine and several boosters with Covid vaccine. While not tested, a flu vaccine and Covid vaccine were mostly given at the same moment.
A recent British study among 1,745 healthcare workers showed booster vaccinations did not contribute to the protection of the healthcare workforce in a post-pandemic setting. The Covid-19 vaccination may even temporarily increase the likelihood of symptomatic infection and workday loss.
Recommending a combined use of four vaccines that prior to use had not been tested together during pregnancy when the immune system is following a precious time clock for the survival of both mother and child has been a risky approach.
Clinical trials with the Covid mRNA vaccine during pregnancy have shown data with serious worries that should have been openly discussed with pregnant women. Moreover, long-term effects for both mother and child remain unknown.
After the Netherlands and the UK, the US only recently said that Covid-19 vaccines are no longer recommended for healthy people under the age of 65 years and pregnant women. Whereas Covid-19 vaccines are still recommended for immunocompromised people, unfortunately they might be more at risk for experiencing Covid-19 infections after booster immunizations.
Although a causal relation remains difficult, the effects of repeated mRNA vaccination in combination or shortly before or after other vaccinations and/or using (psychiatric) medicine need to be elucidated. Sex differences in cost-effective harm analysis will help future decision -making.
Last week Robert F Kennedy, Jr stopped financing 500 million subsidiaries for the mRNA vaccine platform. Also the director of the NIH Dr Jay Bhattacharya wrote an opinion piece for the Washington Post: “Why the NIH is pivoting away from mRNA vaccines.” As a vaccine for a broad public use mRNA technology has failed to earn public trust.
A Post-Pandemic Increase of Female Mortality
In nearly all populations, women live longer than men. The ubiquity of female survival advantage for all ages, even during famine or epidemics, when mortality is extraordinarily high is changing.
Unfortunately, there is limited information available on sex differences in excess mortality from major respiratory infectious diseases. A peer-reviewed study on the first wave of the Covid-19 pandemic in Italy observed that gender differences in excess risk of death existed, but with a nuanced and non-consistent picture. The general finding of this study is that males up to 75 have been suffering more excess deaths as compared to females.
However, this picture is less clear-cut at older ages when more women are living in nursing homes which during the Covid pandemic showed the highest mortality rates. A study from the Netherlands on sex differences in Covid-19 mortalities skipped the data from healthcare workers and people living in nursing homes (mostly females) to confirm that male sex is a predisposing factor for severe Covid-19 independent of age and comorbidities.
Some other studies and a recent study (preprint) suggest Covid-19 did not produce lasting shifts in pre-pandemic sex differences in mortality in High-Income Countries and did not change the fundamental dynamic of the sex mortality gap. The authors observed that the male disadvantage in the Covid-19 mortality based on absolute death counts was concentrated in the pre-vaccine phase and declined over time. Relative increases in mortality were often similar between sexes, and in some cases, greater among women.
Another study on excess mortality of 561 regions and 21 countries in Europe indicate that in many European regions, where drops in life expectancy were more moderate, more pronounced life expectancy losses were found for women. The authors suggest that the degree of mortality deterioration is not necessarily linked to biological sex.
A cohort study of the overall impact of the Covid-19 pandemic on mortality in France observed four consecutive years of excess mortality and a growing impact on people from 20-60s, particularly men.
Unfortunately, no peer-reviewed publications on sex differences and excess mortality cover the years 2024-2025. Yet, during the International Conference of Actuaries in 2025 Nationale Nederlanden, a Dutch insurance company, presented a continued rise in female excess mortality in the Dutch population from 2024-2025, while male excess mortality tended to decline. Furthermore, analysis showed a much higher degree of female excess mortality as compared to EU countries in general, while the Dutch male population experienced a better life expectancy as compared to EU countries.
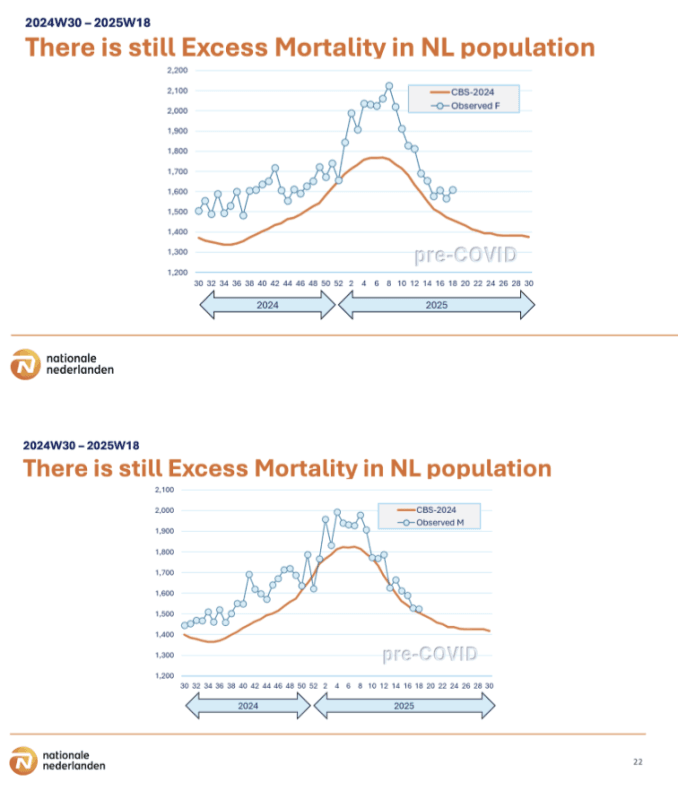
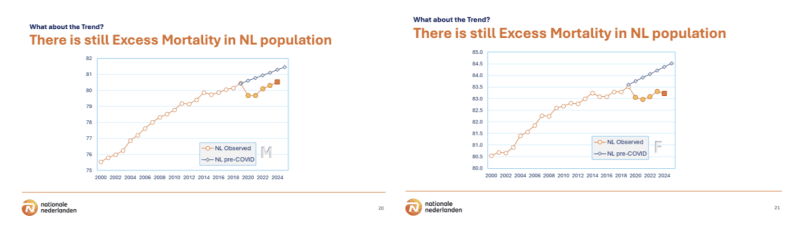
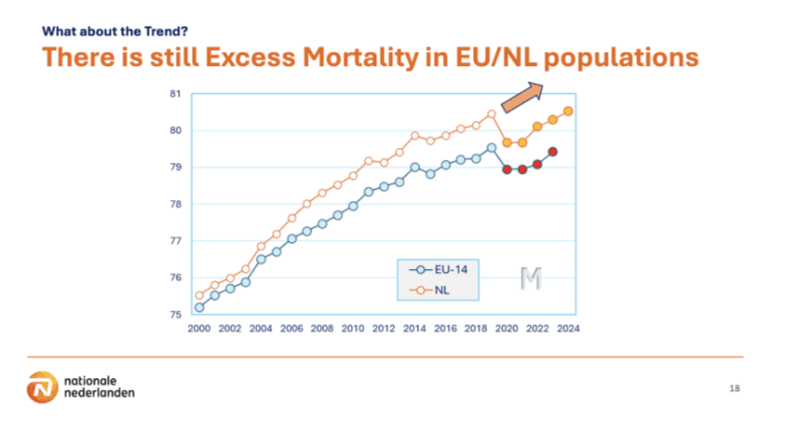
(Source for all of the above images: Presentation 30 years of marketing Dutch Longevity Risk E. Tornij actuary NN The Netherlands. Published with kind permission from E Tornij.
The observation that Dutch females experience poorer health as compared to EU countries is in line with earlier findings. The new update on Eurostat based on data up to 2023 shows a comparable line of unfavorable healthy life years for Dutch women, being 7.8 years (57.5 versus 65.3 years) lower as compared to the mean of all EU countries. In contradiction, Dutch men 2.2 years (60.6 versus 62.8 years) experience far less difference in healthy life years as compared to the mean of all EU countries. The Netherlands is the only EU country where men experience above three years more in healthy life years as compared to women.
Also, England observed that female life expectancy dropped during the Covid-19 pandemic to the lowest among comparator countries (with the exception of the US). Working age mortality rate was 1.5% above the 2015-2019 average. In 2023 the mortality rate was 5.5% above the 2015-2019 average with most of the additional deaths being ‘deaths of despair’ (alcohol, drugs, and suicide). The observed rise in deaths is consistent with an increase in severe mental health problems. Severe mental health problems are more frequently experienced by women and those living in poverty.
A report from LSE International Inequalities Institute showed that austerity measures on healthcare and welfare from 2010-2019 in the UK decreased life expectancy for women nearly double as compared to men. Moreover, the drop in life expectancy developed progressively, indicating a lasting impact that possibly exacerbated during the pandemic and is still at play.
For other High-Income Countries sex difference analysis on excess mortality over the last year has not yet become publicly available. However, data on a continued rise in post-pandemic disabilities and injuries, a forecast for premature deaths, show a higher increase of female claimants for permanent disability awards as compared to the labour force.
The Post-Pandemic Rise in Disability Claims by Women
The article “The Truth Business Leaders Need to Face” published March 2024 documented a more pronounced rise in disabilities in women in various High-Income Countries. Unfortunately, until today the trend with a higher increase of females with disabilities continues in the Netherlands, the UK and the US. Here it is argued that the observed upward trend of a decline in female health in most age groups in the workforce continues today.
The Netherlands
The Netherlands is experiencing a 13% increase in people with disabilities in 2024 as compared to 2023. The number of employees awarded an income provision scheme for fully occupationally disabled (IVA) increased and more employees, especially females (> 60%), received an award after being partially disabled for at least two years, earning 65% or less of their former wage (WGA). Twice as many women as men are outside the labor force. Research has shown that once having been disabled, it is difficult to get back to the same level of job as previously. Furthermore, women experience more barriers to reentering the labor force.
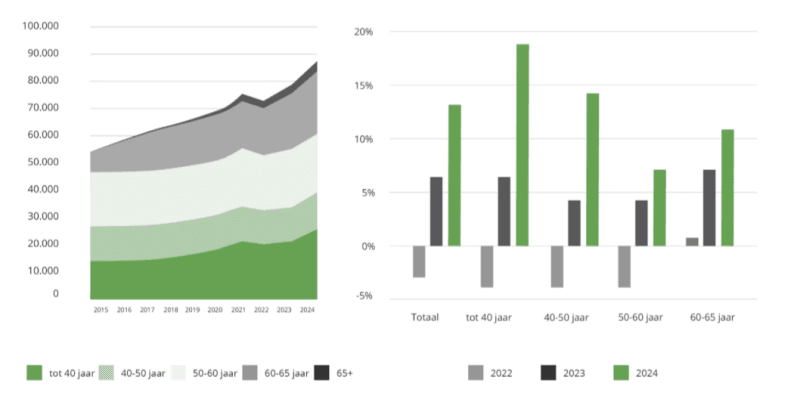
A stunning percentage of 75% of the sharp rise in claimants from 2023-2024 are females. The highest increases are in number of claimants for mental health problems (depression, anxiety, ADHD, and burnout) found in the younger age groups, 16-40 years, predominantly in healthcare and welfare, education, and public administration, with a 24% rise for females and 20% for males. Employees experiencing disabilities with physical problems are steadily declining in the years 2020-2024.
The number of healthcare workers that faced two years sick leave doubled from 2019 to 2024 among all age groups. Until June 2025 long-term illness did not decline.
An increase of people experiencing Long Covid might be another explanation for the rise in WIA claimants in 2024, mostly seen in the age group 50-60 years. The number of claimants increased from 1,500 (2023) to 4,200 (2024) with a sharp spike in the first quarter of 2024. The total number of people experiencing Long Covid symptoms officially registered are 33,429. of which 74.1% is female mostly in the working age group 35-65 years.
UK
An IFS report on PIP analysis in the UK shows new claimants are now more likely to be female than were pre-pandemic. Across all age groups (9,000 additional claims per month amongst those 40-64 years and 7,000 additional claims per month for under 40s), there is a faster growth in new claims for women. The share of new claims made by women has grown from 55% in 2019-2020 to 58% in 2023-2024. For the 2023-2024 claims, there is a bigger share in mental health claims as compared to 2019-2020.
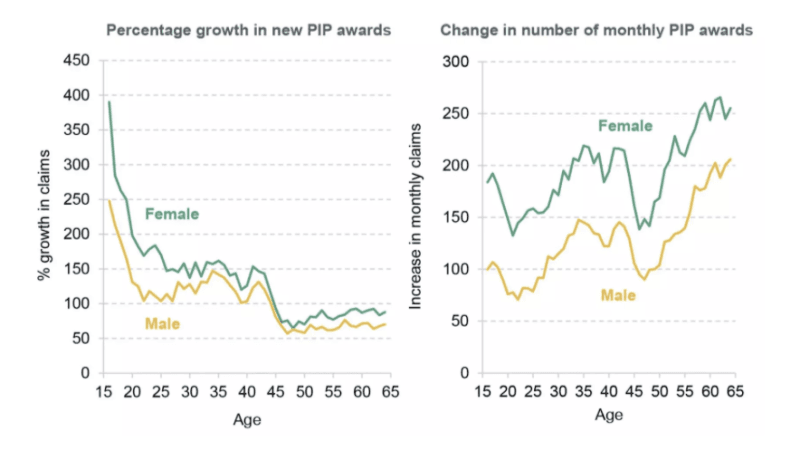
Source: Health-related benefit claims post pandemic: UK trends and global context, Latimer E et al. 19 September 2024.
Sickness absence days per worker were 37 percent higher in 2022 than in 2019, which was evidence to support the argument that population health has worsened. The highest sickness rates were observed at the NHS.
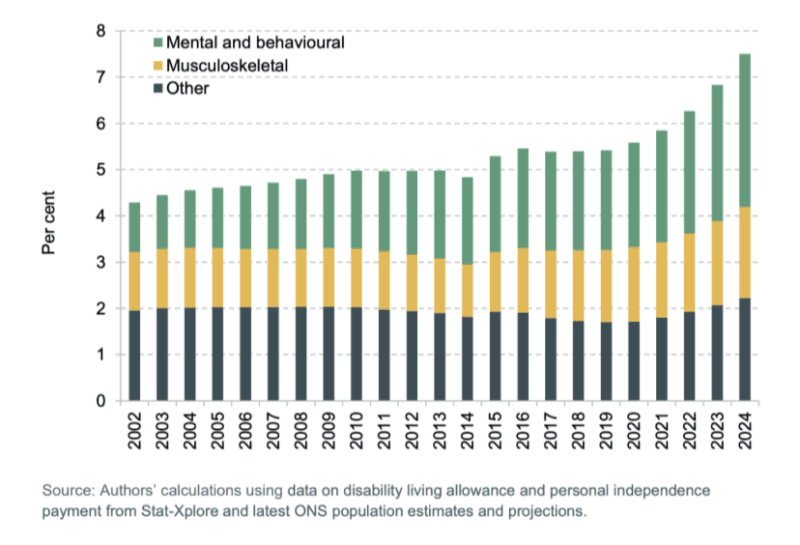
Mental health has worsened since the pandemic. This is consistent with using disability benefit claims for mental health.
During the pandemic, the use of anti-depressants rose by 12% with 8.7 million people in the UK now using them.
Even pre-pandemic studies reveal that antidepressants are the most common medication for women and prevalence of antidepressant use has increased with age. The evidence is there that women who made claims for common medications had a lower socio-economic status.
Stark geographical differences in the prevalence of health-related benefit claims with richer and healthier areas having lower claim rates have been observed repeatedly. People on disability benefits are more likely to be in poverty and material deprivation than working-age individuals in general. An earlier literature review that appeared in 2017 concluded that the impact of austerity measures of policies in the UK was associated with worsening mental health and resulted in increased risk of suicide. From 2012-2019 women’s mortality rates had worsened to a greater degree than men’s mortality rates in the 20% most deprived areas in England, Scotland, and Wales.
US
In the US Civilian labor force, a continuous rise in females with disabilities from 2021 onwards is observed.
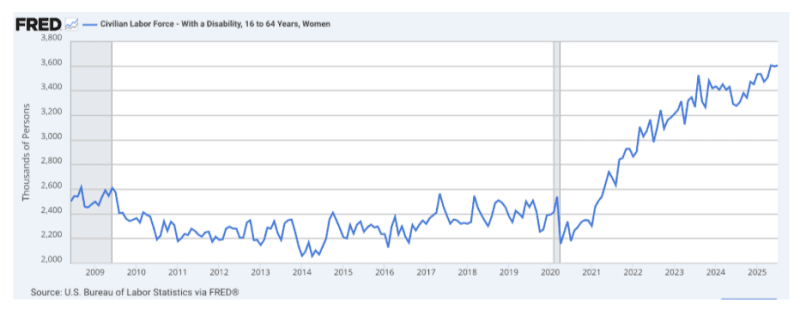
Why the number of claims suddenly started to balloon in 2021 has puzzled many health and policy experts.
According to a study from the US Labor Statistics in 2023, more female workers with disabilities have joined the labor force from late 2021 onwards, which is explained to be a positive effect of the wider adoption of remote work. However, there might be other factors at play with an increasing number of women with mental problems and Long Covid.
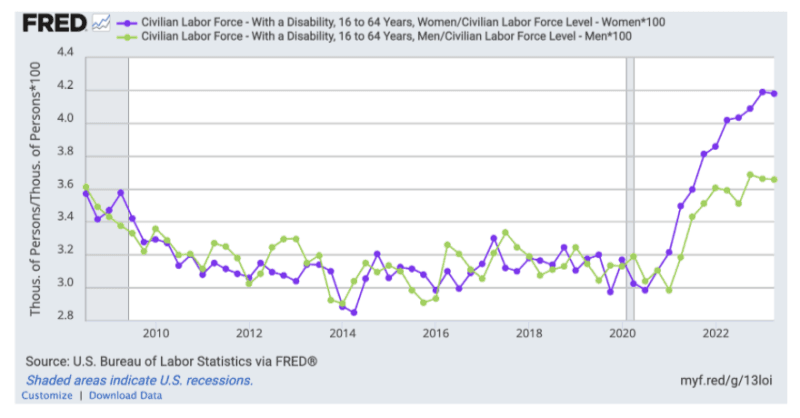
Most of the disabled workers are employed part-time and in many cases are not covered by workplace insurance programs, but do incur higher healthcare bills. The risk to file for a full-time disability benefit is higher for this group.
In many High Income Countries, a relatively high number of people experiencing Long Covid symptoms are unable to work or only for a limited time per week. In the US it is estimated at 15 million people and in the UK 1.9 million. Symptoms (fatigue, difficulty concentration, muscle ache, shortness of breath) that are classified for Long Covid and ME/CFS may also be experienced by people with chronic symptoms/injuries after vaccinations.
Researchers from Yale University recently published their first observations on Post Vaccination Syndrome, a cluster of chronic symptoms that developed soon after Covid-19 vaccination. In the Netherlands the official registered number of people with PVS is 1,234 with 61.9% female, mostly 30-65 years. Real numbers might be much higher.
Different organs may be involved, especially the gut in which 70% of the immune system are located. Currently, there are many publications on chronic mental and physical diseases and cancer that might be related to a dramatic degradation of the human immune system.
A Rapid Decline of the Female Immune System
In the EU, UK, and US leading causes of death are cardiovascular diseases and cancer. During the pandemic both diseases increased in young adults. Whereas a rise in cardiovascular disease is predominantly found in men, the rise in cancer is affecting women most. This seems to be a similar story across the Western world.
In 2024 in the Netherlands, young women 18-39 years were 1.5 times more frequently diagnosed with cancer (breast cancer and cervical cancer) than prostate cancer in young men. Among the EU, the Netherlands ranks number 3 for women diagnosed with cancer
In the UK female cancer rates are set to rise six times faster than in men over the next two decades, and trends are alarming. The title of the annual American Cancer Society Report does not calm the moods either. Cancer mortality continues to drop despite rising incidence in women; rates of new diagnoses under 65 are higher in women than men, especially for those younger than 50 years of age. The progress is jeopardized by increasing incidence for many cancer types, especially among women and younger adults, shifting the burden of disease.
In general, the 5-year relative survival rate has improved in the last 40 years. The only exceptions are uterine (endometrial) cancer and cervical cancer, whose survival rates have declined. The ACS report covers data until 2021. Trend analysis that shows young cancers are up 44%, and that new cancer patients/diagnostics are up 46% may alarm more people. Analysis by Phinance technologies on death trends for neoplasms in the UK and US indicates that from 2021 a novel phenomenon leading to increased neoplasm deaths appears to be present in individuals aged 15-44 years.
By 2035 cancer is predicted to become a leading cause of death in the EU. The WHO warns cancer cases will jump 77% by 2050.
Although viewed as distinct diagnoses, cancer and cardiovascular diseases are associated with shared risk factors and common pathophysiological pathways. A new study published in Nature suggests that sleeping cancer cells can be roused by Covid and Flu virus. With reflection to another recent peer-reviewed article published in Nature that Covid-19 mRNA booster vaccinations increase flu-like symptoms in healthcare workers, there is a serious warning.
A study on global data consistently observed Flu vaccines and Covid-19 mRNA vaccines among five drugs with myocarditis or pericarditis. Other factors such as declined access to healthcare, changes in nutrition and lifestyle behavior during the pandemic, and post-pandemic economic instability may play a role as well.
A dysregulated immune system and gut dysbiosis might be involved in many other diseases as well.
Post-2020, increased infectious diseases, cardiovascular diseases, turbo-cancer and unusual metastasis of colon, liver, and pancreas, muscular diseases, eye problems, neurological disorders, autoimmune disorders (80% female), acute kidney injury, Long Covid (73% female), mental health problems (> 60% female), and increased memory problems among people in their 30s and 40s are observed.
The increasing number of females living with at least one chronic condition even at a young age needs to reverse. A key indicator of chronic disease burden is the role in driving mortality and long-term care needs with a high fiscal impact.
In the Netherlands the yearly costs on disabilities have reached €28.7 billion/year. It is expected to stabilize in the next few years. However, the UK disability bill is expected to exceed £100 billion by 2029-2030.
The estimated value of health loss during Covid-19 for the US is about 48% of US GDP ($8.5 trillion). Health loss during the pandemic included premature death, long-term health impairment, and mental health impairment. Mortality cost of the pandemic has been estimated to be about 33% of the global income.
A Global Public Health Policy Towards Better Female Health
The continued rise in female excess mortality and disabilities can’t be neglected.
For decennia, Public Health Experts, policy makers, and CEOs of insurance companies have been aware of the benefits of prevention, but have rather invested in medicalization and low healthcare, with welfare worker salaries hitting female health the most. With declining revenue and being obliged to deliver the healthcare and quality of care insured people need and pay for, insurance companies have no escape.
Instead of austerity measures, the moral thing to do is investments for better female health that will boost a population’s health and secure economic stability that is needed most.
To start and secure an upward trend a public health policy for better female health:
- Boost health, prevent and reverse disease through personalised nutrition and lifestyle using the best of ancient knowledge and modern medicine to restore the immune system.
- Addressing overmedicalization and overdiagnosis of women, especially during pregnancies and pre-pregnancies.
- Approved medicine without placebo-controlled trials in women will receive a box safety warning for women and is discussed by medical doctors in shared decision-making and prescription (informed consent).
- Not safe and effective for women is taken seriously. Side effects of vaccines or medicine reported by women are noticed in safety systems and act upon for withdrawal of medicine from the market when proven to be a risk, not safe and effective for women.
- Gender equal payments and a living salary for women in the lowest paid jobs to allow a decent independent living able to buy healthy nutrition and pay for sufficient energy and clean water supply.
- Zero tolerance for mental and physical abuse of women at the workplace and in society.
Improving healthy aging is a fundamental objective of human activity and leads to lower public health expenditures. This will increase the possibility that people continue to work later into life. Many countries are facing a demographic cliff with declining birth rates. A global public health strategy to better female health is a strategy for economic stability.
A Hidden Post-Pandemic Increase in the Decline of Female Health
by Carla Peeters at Brownstone Institute – Daily Economics, Policy, Public Health, Society
Author: Carla Peeters
This content is courtesy of, and owned and copyrighted by, https://brownstone.org and its author. This content is made available by use of the public RSS feed offered by the host site and is used for educational purposes only. If you are the author or represent the host site and would like this content removed now and in the future, please contact USSANews.com using the email address in the Contact page found in the website menu.








