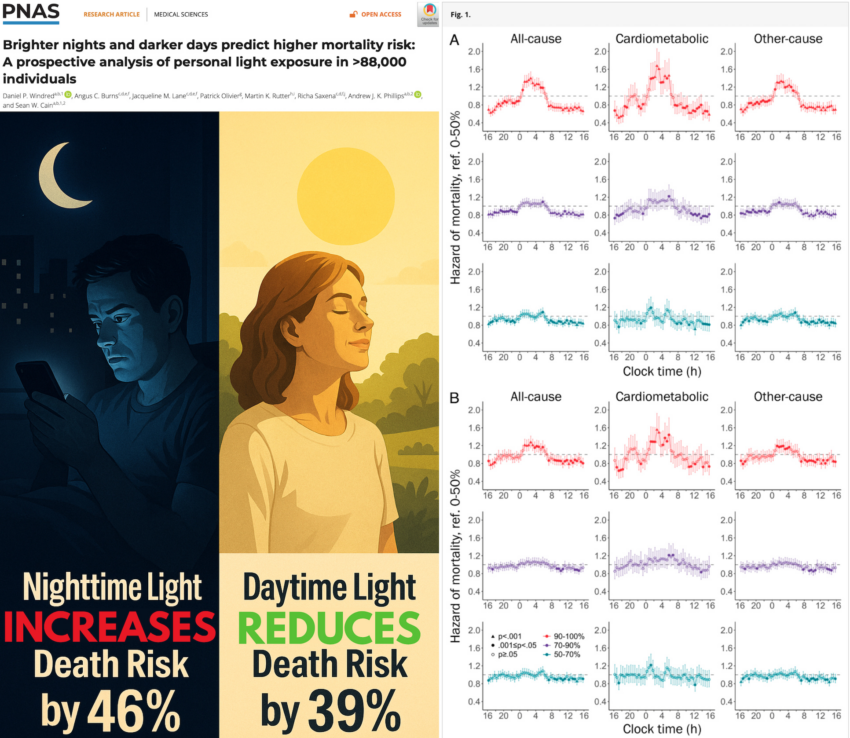
A groundbreaking study published in PNAS titled, Brighter nights and darker days predict higher mortality risk: A prospective analysis of personal light exposure in >88,000 individuals, has provided the strongest evidence to date that how much light we are exposed to—both during the day and night—directly impacts our lifespan.
Using objective data from over 88,000 adults who wore wrist-based light sensors continuously for 7 days—capturing more than 13 million hours of personal light exposure—and tracking their health outcomes over nearly a decade, the study found that brighter light at night and dimmer light during the day are associated with significantly higher risks of all-cause and cardiometabolic mortality.
Study Design
-
Cohort: 88,905 UK Biobank participants, average age 62.4, 57% female
-
Light Data: Wrist-worn light sensors (Axivity AX3) worn for 7 consecutive days, collecting over 13 million hours of data
-
Analysis: Light exposure was divided into percentiles for day (07:30–20:30) and night (00:30–06:00). Circadian phase and amplitude were modeled using a biologically validated algorithm.
-
Outcomes: Cause-specific mortality tracked over 8 years, totaling 3,750 deaths (798 cardiometabolic)
Three levels of statistical adjustment were used to control for age, sex, ethnicity, season, employment, income, physical activity, smoking, alcohol use, urban vs. rural living, and social behaviors.
Key Findings
1. Nighttime Light Increases Mortality Risk
Participants exposed to the brightest night light (top 10%) had:
-
21–34% higher risk of all-cause mortality
-
33–46% higher risk of death from cardiometabolic diseases
This risk followed a clear dose–response pattern: the more nighttime light, the greater the risk.
2. Daytime Light Reduces Mortality Risk
Conversely, participants with the highest daytime light exposure had:
-
Up to 34% lower risk of all-cause mortality
-
39% lower risk of cardiometabolic mortality compared to those with the lowest daytime light
This again followed a graded, dose-responsive trend.
3. Disrupted Circadian Rhythms Predict Death
Using a validated mathematical model of the human circadian pacemaker, researchers showed:
-
Lower circadian amplitude (a weaker internal clock signal) predicted up to 10% higher all-cause mortality and up to 13% higher cardiometabolic mortality
-
Both early and late circadian phases—deviations from the average sleep-wake timing—were associated with significantly increased death risk
These relationships held even after adjusting for sleep duration and efficiency, indicating that circadian disruption itself is an independent risk factor.
Implications
This is the largest prospective study to directly measure personal light exposure and link it to mortality. Unlike prior studies using satellite or self-reported data, it captures the true lived light environment—indoors and out. The findings corroborate prior research showing that light at night disrupts circadian rhythms, contributing to metabolic, cardiovascular, and endocrine dysfunction.
The findings have profound implications:
-
Brighter nights (due to indoor lighting, screens, or urban exposure) may be silently shortening lifespans
-
Dim daytime environments (e.g., indoor office work) fail to reinforce circadian strength and resilience
-
Circadian health—including consistent light–dark exposure—is emerging as a major determinant of human longevity
Advice
-
Avoid bright light exposure between midnight and 6 a.m., when the circadian system is most vulnerable
-
Increase bright light exposure during the day, especially in the morning hours
-
Maintain regular sleep-wake patterns and minimize artificial light at night, including screens and ambient indoor lighting
These behavioral changes are low-cost, accessible, and evidence-based strategies to possibly reduce premature mortality risk and support cardiometabolic health.
Epidemiologist and Foundation Administrator, McCullough Foundation
www.mcculloughfnd.org
Please consider following both the McCullough Foundation and my personal account on X (formerly Twitter) for further content.
Click this link for the original source of this article.
Author: Nicolas Hulscher, MPH
This content is courtesy of, and owned and copyrighted by, https://petermcculloughmd.substack.com and its author. This content is made available by use of the public RSS feed offered by the host site and is used for educational purposes only. If you are the author or represent the host site and would like this content removed now and in the future, please contact USSANews.com using the email address in the Contact page found in the website menu.