By SRH,
Ensuring safety and effectiveness: A significant development has occurred as the Japanese Ministry of Health has raised the budget for COVID vaccine health damage by 110 times from previous estimates. Anticipating a significant number of fatalities, also known as severe health consequences.
Reliable and efficient An astonishing development has been reported by the Japanese Ministry of Health, revealing that the health harm budget for the COVID vaccine in Japan has surged by 110 times from previous estimates. Anticipating a significant number of fatalities or illnesses.
The Japanese Ministry of Health has significantly increased the budget for COVID vaccine health damage compared to previous estimates. There is a high anticipation of significant health consequences!
Regarding the foundation, it pertains to the budget for health damages caused by the new coronavirus vaccine in the FY2025 fiscal year.
This budget was initially set at 360 million yen. However, the supplementary budget revealed a total of 39.77 billion yen.
It’s been reported that the Ministry of Health, Labour, and Welfare now estimates health damage incidents to be 110 times larger than previously thought. There has been a significant increase in the COVID vaccine health damage budget by the Japanese Ministry of Health, now 110 times higher than previous estimates. There is a significant concern about potential health impacts!
Regarding the foundation, it pertains to the budget for health damages caused by the new coronavirus vaccine in the FY2025 fiscal year.
The initial budget was 360 million yen. Surprisingly, the supplementary budget ended up being 39.77 billion yen.
It’s been reported that the Ministry of Health, Labour, and Welfare now estimates health damage incidents to be 110 times larger than previously thought.
We really appreciate your help. Maintaining the websites and live streaming videos requires a substantial financial commitment. Any amount contribution is much appreciated. Please think about contributing a reasonable amount on a monthly basis.
Please Give Please Give
You can also send a check to PO Box 127, Pontotoc, TX 76869.
The HIMEDIA Group.
Side Bar:
Throughout 2021, excess deaths were far higher than they were in 2020 except for weeks 29 and 30.
Unfortunately, official figures provided by the CDC show that the trend continued through 2022.
The most recent data released by the CDC covers up to week 40, the week ending October 9.
The CDC has confirmed that there have been 7,680 more excess deaths among children and young adults in 2022 so far than there were during the same time frame in 2020 at the height of the Covid pandemic, according to a report from the Exposé.

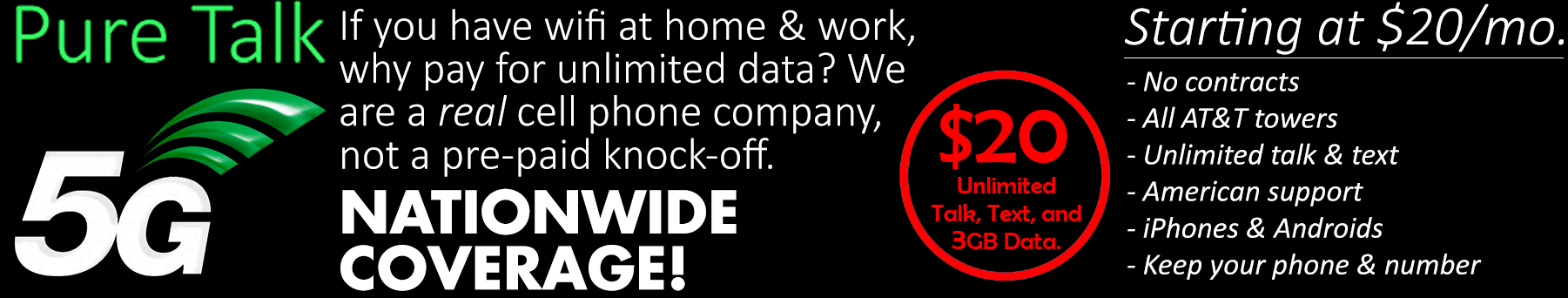
Slim sized Perfume Oils are perfect to take with you in your hand bag, gym bag, or for traveling. Roll a small amount on your pulse points. These are very concentrated, absorb quickly, and last a long time. www.graniteridgesoapworks.store
Revelation: A Blueprint for the Great Tribulation
A Watchman Is Awakened


Will Putin Fulfill Biblical Prophecy and Attack Israel?
Newsletter
Orphans

Editor’s Bio

A Thrilling Ride
Every once in awhile, a book comes across your path that is impossible to put down. A Long Journey Home is not a casual book that you read in a week or earmark to complete at a later date. Once you begin, cancel your schedule, put your phone on silent, find a quiet place where you cannot be disturbed, and complete the journey. Click Here to Purchase on Amazon.com!
Recent News

Get Prepared From HNewsWire
The post Watchman: Safe and Effective the Health Harm Budget for the COVID Vaccine in Japan Was Boosted by an Astounding 110 Times When Compared to Earlier Predictions, According to the Watchman A Large Number of Deaths, or Illnesses, Is What They Expect and It’s Coming! appeared first on www.HNewsWire.com.
Click this link for the original source of this article.
Author: StevieRay Hansen
This content is courtesy of, and owned and copyrighted by, https://hnewswire.com and its author. This content is made available by use of the public RSS feed offered by the host site and is used for educational purposes only. If you are the author or represent the host site and would like this content removed now and in the future, please contact USSANews.com using the email address in the Contact page found in the website menu.